Does your joint pain impact you getting on with living, exercising, working? Is it worse on waking? Does it leave you feeling tired and wanting to regain your vitality? Perhaps you have tried things to help alleviate the pain and increase mobility (e.g. heat, relaxation techniques, yoga) Do you experience any digestive issues too? Maybe you have already made some dietary changes.
Rheumatoid arthritis (RA)
Rheumatoid arthritis (RA) symptoms include joint pain, swelling and stiffness and can lead to reduced joint mobility (1). RA is a chronic inflammatory autoimmune condition mainly in the peripheral joints, such as hands, elbows, knees. It affects about 0.5-1% of the adult population worldwide (2). Known risk factors are genetics, gender (more prevalent in females), age (from circa 50 years) and smoking (3,4).
Getting control over your symptoms isn’t easy. It takes time to identify and understand the triggers for you personally and learn new food choices and habits that can help and support you. A nutritional therapy approach with a nutrition practitioner would be personalised, i.e. depend on your specific symptoms, guide and educate you to manage your body and would be done in partnership with your GP, medication and other aspects of the condition to manage. You can learn what works for your body so that you can get on with living.
The research shows nutrition factors such as plant based eating, eating gluten free (2), probiotic supplements (3,5,6), and a Mediterranean diet (7) can help reduce symptoms of RA and be a complementary approach in combination with RA medication(s). There is scientific evidence to show that the types and levels of bacteria in the digestive system is different with RA, i.e. there are specific RA-associated bacteria (8–10) that can play a role in the inflammatory nature of this condition. Weakness in the lining of the intestinal wall can mean bacteria leak out which may increase inflammation in the RA condition (11,12).
Nutritional therapy can help rebalance the bacteria in the digestive system and support strengthening the intestinal wall lining with both dietary changes and supplements if appropriate. Probiotic supplements have been shown to improve overall wellbeing in RA patients and in some studies specific probiotic strains (for example Lactobacillus Casei 01 found in some dairy products) reduced inflammation and ameliorated RA symptoms such as joint swelling (5,6,13).
Examples of nutritional recommendations for RA
- reducing joint and muscle pain by reducing inflammation and immune responses with an anti-inflammatory dietary approach
- addressing tiredness and brain fog by balancing blood sugar in all meals and snacks
- reducing tension by addressing stressors, both physical and emotional
- addressing joint pain, exercise recovery, muscle weakness, low energy with nutrient sufficiency, not just the recommended government guideline but personalised levels for your body
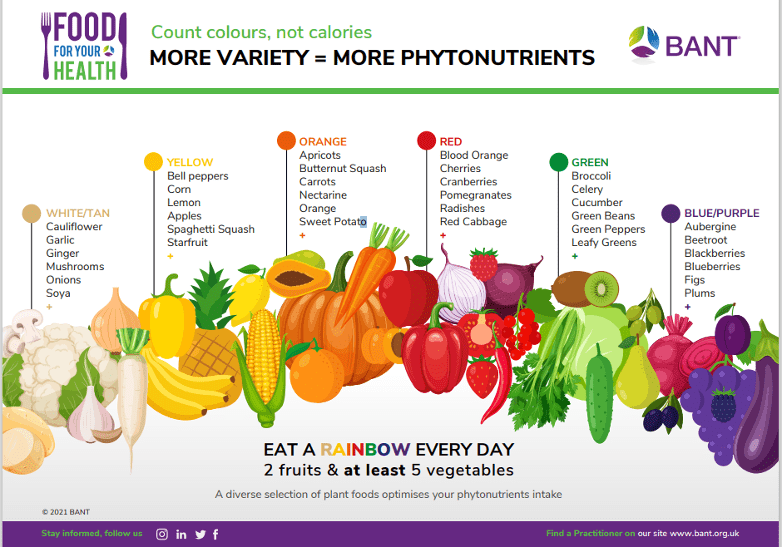
- reducing joint and muscle pain and digestive issues with digestive system support and bacteria balancing by “eating the rainbow” (i.e. eating a wide variety of foods, mostly plants – see below) and regularly eating some (not too much!) prebiotic and probiotic foods. They support the growth and maintenance of good bacteria levels for digestive health, immunity, vitamin and energy synthesis, and regulation of inflammation. Probiotics are fermented foods such as yoghurt, kefir and kombucha and can be both dairy and non-dairy. Prebiotic foods are garlic, onion, leeks, beans, peas, artichoke, chicory, apples, bananas, and wholegrains.
References
- Hamel K, Doodes P, Cao Y, Wang Y, Martinson J, Dunn R, et al. Suppression of Proteoglycan-Induced Arthritis by Anti-CD20 B Cell Depletion Therapy Is Mediated by Reduction in Autoantibodies and CD4 + T Cell Reactivity . J Immunol. 2008;180(7):4994–5003.
- Alwarith J, Kahleova H, Rembert E, Yonas W, Dort S, Calcagno M, et al. Nutrition Interventions in Rheumatoid Arthritis: The Potential Use of Plant-Based Diets. A Review. Front Nutr. 2019;6(September):1–11.
- Lerner A, Matthias T. Rheumatoid arthritis-celiac disease relationship: Joints get that gut feeling. Autoimmun Rev [Internet]. 2015;14(11):1038–47. Available from: http://dx.doi.org/10.1016/j.autrev.2015.07.007
- Gomez A, Luckey D, Yeoman CJ, Marietta E V., Berg Miller ME, Murray JA, et al. Loss of sex and age driven differences in the gut microbiome characterize arthritis-susceptible *0401 mice but not arthritis-resistant *0402 mice. PLoS One. 2012;7(4).
- Alipour B, Homayouni-Rad A, Vaghef-Mehrabany E, Sharif SK, Vaghef-Mehrabany L, Asghari-Jafarabadi M, et al. Effects of Lactobacillus casei supplementation on disease activity and inflammatory cytokines in rheumatoid arthritis patients: A randomized double-blind clinical trial. Int J Rheum Dis. 2014;17(5):519–27.
- Zamani B, Golkar HR, Farshbaf S, Emadi-Baygi M, Tahabadi-Ebrahimi M, Jafari P, et al. Clinical and metabolic response to probiotic supplementation in patients with rheumatoid arthritis: a randomized, double-blind, placebo-controlled trial. Int J Rheum Dis. 2016;19:869–879.
- Guerreiro CS, Calado Â, Sousa J, Fonseca JE. Diet, microbiota, and gut permeability-the unknown triad in rheumatoid arthritis. Front Med. 2018;5(DEC):1–7.
- Scher JU, Sczesnak A, Longman RS, Segata N, Ubeda C, Bielski C, et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife. 2013;2:1–20.
- Zhang X, Zhang D, Jia H, Feng Q, Wang D, Liang D, et al. The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat Med [Internet]. 2015;21(8):895–905. Available from: http://dx.doi.org/10.1038/nm.3914
- Maeda Y, Kurakawa T, Umemoto E, Motooka D, Ito Y, Gotoh K, et al. Dysbiosis Contributes to Arthritis Development via Activation of Autoreactive T Cells in the Intestine. Arthritis Rheumatol. 2016;68(11):2646–61.
- Chen J, Wright K, Davis JM, Jeraldo P, Marietta E V., Murray J, et al. An expansion of rare lineage intestinal microbes characterizes rheumatoid arthritis. Genome Med [Internet]. 2016;8(1):1–14. Available from: http://dx.doi.org/10.1186/s13073-016-0299-7
- Jubair WK, Hendrickson JD, Severs EL, Schulz HM, Adhikari S, Ir D, et al. Modulation of Inflammatory Arthritis in Mice by Gut Microbiota Through Mucosal Inflammation and Autoantibody Generation. Arthritis Rheumatol. 2018;70(8):1220–33.
- Vaghef-Mehrabany E, Alipour B, Homayouni-Rad A, Sharif SK, Asghari-Jafarabadi M, Zavvari S. Probiotic supplementation improves inflammatory status in patients with rheumatoid arthritis. Nutrition [Internet]. 2014;30(4):430–5. Available from: http://dx.doi.org/10.1016/j.nut.2013.09.007
Disclaimer: This information is explanatory in nature and/or provides general dietary advice. It is not personalised nutritional and lifestyle recommendations since no health history has been recorded.